Curriculum
The residency curriculum has recently been restructured to accommodate for the new board exam as well as the re-structured mini-fellowship format of 4th year. Residents rotate in a series of two-week or four-week blocks in the following subspecialty areas:
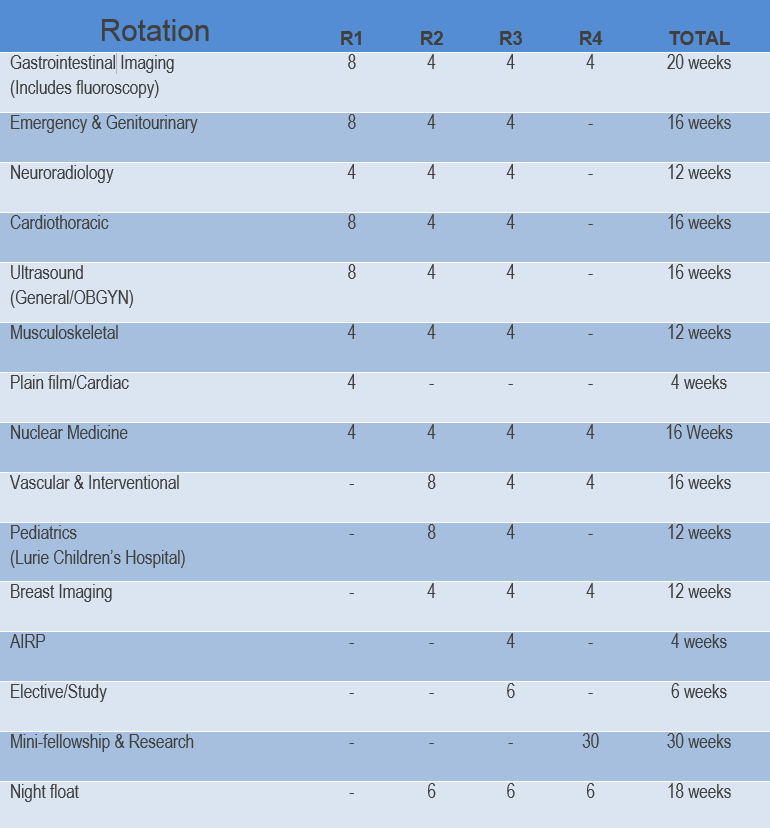
(Number of weeks per rotation)
Rotations
Emergency Radiology:
The call system is covered through a rotating night float system, with daytime Emergency Department coverage provided by a dedicated ER resident. As a busy level 1 adult and pediatric trauma center, hands on experience is extensive.
Residents read and interpret all cross-sectional imaging from the Emergency Department and gain experience in a full spectrum of acute pathology, including neuroradiology, body CT/MR, and musculoskeletal imaging.
Genitourinary
Residents receive hands on experience in standard methods of urography, including intravenous pyelography, CT and MRI. A joint project with the Department of Urology provides training in ultrasound guided prostate biopsy – a unique offering at Illinois Masonic Medical Center.
As part of the Emergency Radiology rotation, residents also become proficient in GU fluoroscopy, including voiding cystourethrograms and hysterosalpingograms.
Gastrointestinal Imaging:
A large volume of diverse cases provide residents ample opportunity to become proficient in interpreting abdominal and pelvic CT and MRI, including cholangiopancreatography (MRCP).
State-of-the-art digital fluoroscopy suites are a special feature of our program. Residents receive extensive hands-on training in fluoroscopy technique and perform all gastrointestinal fluoroscopic studies.
Neuroradiology:
Residents receive extensive training in a wide spectrum of acute and non-acute central nervous system pathology. Modalities include CT, MRI, angiography, and myelography in a high volume clinical setting. As a level I trauma center, residents receive intense exposure to trauma and emergent cases. Illinois Masonic is also home to a Neurosciences Institute and Comprehensive Spine Center, providing residents ample neuroradiology exposure. Additionally, residents assist in all lumbar punctures, vertebral body biopsies, and diagnostic cerebral angiograms.
Cardiothoracic:
Cardiothoracic imaging is a high volume section, with over 40,000 chest examinations performed annually. Residents receive training in all thoracic and cardiac imaging modalities, including CT, high-resolution CT, angiography, cardiac CT, and cardiac MRI.
Ultrasound:
Residents receive dedicated training in performing and interpreting general abdominal, obstetrical, and gynecological studies. Residents are well trained in interpretation of first trimester obstetrical ultrasound and receive training in second and third trimester ultrasound by spending one day a week during their rotation at the outpatient antenatal clinic at Illinois Masonic. In addition, residents also become proficient in ultrasound-guided thyroid biopsies and hysterosonograms during this rotation.
Musculoskeletal:
Our high volume level I trauma center provides residents extensive exposure to musculoskeletal trauma. In addition, residents read and interpret over 100 joint MRI examinations during each rotation. Modalities include plain film, CT, and MRI. In addition, residents become well trained in musculoskeletal fluoroscopy, including arthrography and joint aspirations.
Nuclear Medicine
As required by the ACGME, residents receive 16 weeks of nuclear medicine training, with 8 weeks provided through 2 separate one-month rotations at Loyola University during the 3rd and 4th years. All residents are appropriately trained to receive full Authorized User (AU) status through the Nuclear Regulatory Commission (NRC) and receive training in basic nuclear medicine, SPECT, and PET/CT. Special features include attenuation correction and gated SPECT for cardiac imaging as well as PET/CT fusion. Residents also participate in a variety of nuclear medicine procedures, including radioiodine therapies and lymphoscintigraphy.
Vascular/Interventional:
Residents learn patient management and gain exceptional hands-on training experience as first assist in a wide variety of procedures including tissue biopsy, diagnostic angiography, angioplasty, stent and graft placement, GU, GI and biliary interventions, dialysis fistula management, TIPS, uterine fibroid embolization, radioembolization, and endovenous ablation. Resident experience is enhanced by the lack of an IR fellow.
In addition, residents read and interpret CT angiography as well as non-invasive vascular imaging including arterial and venous Doppler, lower extremity relux examinations, and carotid ultrasound.
Pediatrics: Residents spend a total of 8 months during their second and third years at Lurie Children's Hospital, where they receive dedicated pediatric training in plain film, ultrasound, CT, MRI, and fluoroscopy. In addition, dedicated pediatric lectures are provided by a fellowship-trained pediatric guest lecturer on a bi-monthly basis.
Breast Imaging:
Residents rotate in our outpatient Women’s Imaging Center learning basic and advanced breast imaging, including screening and diagnostic mammography, ultrasound, and magnetic resonance imaging. In addition, residents participate as first assist in all breast procedures, including core biopsy, needle localization, and ductography.
American Institute for Radiologic Pathology:
Residents attend a four-week radiologic pathology correlation course, sponsored by the American College of Radiology (ACR) during their third year as part of their board preparation. Illinois Masonic provides full tuition and housing for residents to attend.
Research:
Clinical research opportunities relating to all disciplines of radiology are available and encouraged. At minimum, participation in one research project is required to successfully complete the residency program. Dedicated research time is provided to all interested residents during the second through fourth years.
