Chronic acid reflux (Gastroesophageal reflux disease)
If acid reflux disease – also known as gastroesophageal reflux disease (GERD) – is affecting your life, our experts can help you control it before it damages your health. We can also determine whether your GERD has progressed to Barrett's esophagus – a serious, precancerous condition – so you can get necessary acid reflux treatments as quickly as possible.
Have a referral to a gastroenterologist to discuss GERD symptoms? Schedule an appointment by calling 800-3-ADVOCATE or use our online search to find a gastroenterologist near you.
What is acid reflux?
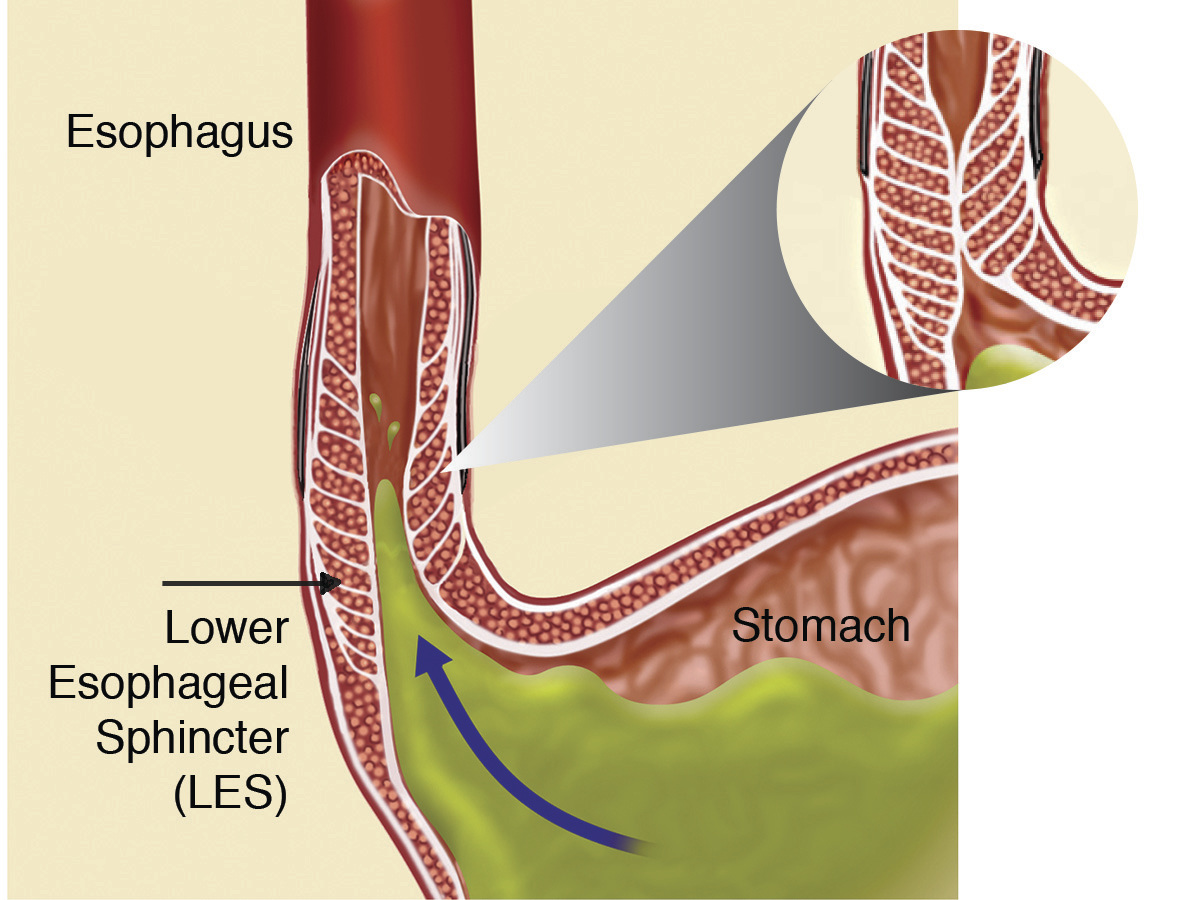
Acid reflux happens when acid and bile from the stomach back up into the bottom of the esophagus (the tube that connects your mouth and your stomach). A muscle at the bottom of the esophagus is supposed to open to let food pass into the stomach and then close to keep food in the stomach. When the muscle relaxes too often or too long, acid and bile can flow back into the esophagus.
While the lining of your stomach is intended to handle acid and bile, the lining of the esophagus can be damaged by such reflux. When you have acid reflux, it causes a burning feeling that’s called heartburn or acid indigestion.
Occasional heartburn can be treated at home with over-the-counter remedies. Chronic or persistent heartburn is called gastroesophageal reflux disease (GERD) and it needs more comprehensive acid reflux treatments.
GERD symptoms
There's more to GERD than regular heartburn. When it becomes chronic, it can also cause any of these symptoms.
- Chest pain (severe chest pain could be something more serious than GERD and requires immediate medical help)
- A sour taste in the mouth
- Difficulty or pain when swallowing
- Regurgitation
- Belching
- Bloating
- Nausea
- Wearing away of tooth enamel
- Shortness of breath
- Asthma
- Dry cough or repeated throat clearing
- Sore throat, hoarseness or laryngitis
When an infant has acid reflux, they have different symptoms than an older child or an adult. It can lead to fussiness and arching during feedings along with other symptoms. They may spit up a lot and even vomit. Sometimes babies with acid reflux fail to gain weight as they should, so it’s important to consult your pediatrician as soon as possible.
If you have any of the following symptoms, you may already have serious damage in your esophagus and you should contact your doctor immediately.
- Severe chest pain
- Difficulty swallowing or a feeling that food is trapped
- Bleeding, vomiting blood, or having bloody or tarry, black bowel movements
- Choking: a sensation of acid refluxed into the windpipe (from the top of the esophagus) causing shortness of breath, coughing or hoarseness of the voice
- Unexplained weight loss
What helps acid reflux & occasional heartburn?
Usually, acid reflux or occasional heartburn can be helped by lifestyle changes and using over-the-counter acid reflux medicine.
Lifestyle changes for acid reflux treatments
We can help you with lifestyle changes that could ease your symptoms.
- Quitting smoking
- Limiting fried and fatty foods, peppermint, chocolate, alcohol, citrus fruits, tomato-based foods, caffeine, and carbonated drinks
- Eating smaller portions and avoiding overeating
- Losing weight, if necessary
- Limiting consumption of alcohol
- Waiting two to three hours after a meal to lie down or go to bed
- Elevating the head of your bed by six inches or using a pillow wedge to raise the angle of your head and neck while you sleep
Over-the-counter acid reflux medicines
Many over-the-counter medicines are available to treat occasional heartburn. They include acid reflux medicines that neutralize acid in the stomach, block the flow of stomach contents into the esophagus or decrease fluids produced in the stomach.
These acid reflux medicines work well for people who have heartburn sometimes. But if you find yourself using them more than twice a week, you should contact your doctor. Chronic heartburn can damage the esophagus lining, narrow or cause an obstruction of the esophagus, or contribute to Barrett’s esophagus.
GERD risk factors
The following factors may contribute to GERD.
- Being overweight
- Eating large meals or overeating
- Consuming citrus fruits, tomato-based foods, chocolate, caffeine, alcohol, carbonated drinks, peppermint, or fatty or spicy foods
- Smoking
- Pregnancy
- Having a hiatal hernia
- Using nonsteroidal anti-inflammatory drugs such as aspirin and ibuprofen
Find the right treatment plan for GERD
GERD treatment starts with an accurate diagnosis. Your doctor will perform a physical exam and may order tests such as these:
- Endoscopy: During this procedure, an endoscope (a flexible tube with a light and a tiny camera) is inserted down your throat to examine the esophagus and stomach. A biopsy (tissue sample) may also be taken.
- pH monitoring: A test that checks for stomach acid in the esophagus.
- Motility testing: A procedure that tests whether the muscles of the esophagus are working correctly.
Treating GERD successfully might involve making lifestyle changes like those listed above, taking medication or having surgery. Our experts will work with you to develop an individualized GERD treatment plan based on:
- Your age, overall health and medical history
- Extent of the condition
- Your tolerance for specific medications, procedures or therapies
- Your expectations and preferences
Medications for GERD
Along with lifestyle changes, your doctor may suggest over-the-counter medication.
Common GERD medications:
- Antacids: Over-the-counter medicines that neutralize acid already in the stomach.
- H2 blockers: Medicines that reduce acid production.
- Proton pump inhibitors(PPIs): Medications that effectively stop acid production. Prescription-strength PPIs are commonly prescribed and are often very effective in treating the side effects of GERD, including heartburn, but they don't treat the underlying cause. Long-term use may also cause side effects.
If over-the-counter medication doesn't work, your doctor may recommend prescription-strength versions of H2 blockers or proton pump inhibitors. Or they may prescribe prokinetic agents to tighten the muscle between the stomach and esophagus (esophageal sphincter) and help your stomach empty faster.
Surgery for GERD
For most people with acid reflux, medications help reduce symptoms. But they don’t work for everyone, and they don’t repair the underlying cause of GERD.
When is surgery right for you?
For moderate or severe acid reflux, surgery may be a treatment option if you:
- Continue to suffer from persistent heartburn or other reflux symptoms while taking medication
- Develop or are concerned about developing adverse side effects from taking medication
- Experience your symptoms returning when you stop medication therapy
- Have a damaged esophagus including bleeding or a narrowing (stricture) of the esophagus
- Prefer not to take lifelong medication or can't afford medication long-term
Our experts specialize in minimally invasive acid reflux treatments.
- Fundoplication surgery
- LINX Reflux Management System
Advanced care for Barrett’s esophagus
Barrett’s esophagus is a precancerous condition that's been associated with chronic GERD. It occurs when the esophagus is exposed to acid reflux over a long period of time. As the stomach acid degrades the esophageal lining, it becomes inflamed and infected. Over time, cancerous cells can form.
Innovative treatment
We specialize in endoscopic radiofrequency ablation therapy. This highly effective procedure is a less invasive alternative to traditional surgery that has revolutionized the treatment of Barrett’s esophagus. Previously, Barrett’s esophagus was managed with watchful waiting followed by traditional surgery. Through radiofrequency ablation therapy, our experts can burn away the diseased esophageal lining to make way for the growth of healthy tissue.
How endoscopic radiofrequency ablation therapy works:
Radiofrequency ablation therapy is an outpatient procedure that takes less than an hour. Our experts use an endoscope (a tube-shaped device with a fiber-optic light and camera at the end) to visually examine the esophagus. No incisions are needed.
- First, while the patient is sedated, the doctor passes the endoscope through the patient’s mouth and guides it down the esophagus.
- The doctor then uses the endoscope to insert a catheter that generates short bursts of high energy around the circumference of the esophagus. This will burn away a thin layer of the damaged tissue.
- Within three to four weeks, new, healthy tissue replaces the affected Barrett’s tissue for most patients.
- Following the procedure, patients resume medications for acid suppression.
Recent studies show that 90 percent of patients treated with radiofrequency ablation have no residual Barrett’s esophagus tissue three years after treatment.
Do you suffer from acid reflux?
Millions of people suffer from acid reflux, more commonly known as heartburn. Our acid reflux quiz evaluates your symptoms, identifies your risk factors and gives you an idea of what to do next based on your results.
Get care
We help you live well. And we’re here for you in person and online.