Bronchodilator therapy
Bronchodilator therapy may be recommended for you when you have an allergy or a disease of the lungs such as asthma or chronic obstructive pulmonary disease (COPD). Your Advocate specialist will work with you to find a medication to keep your lungs working as well as they can.
What is bronchodilation?
Bronchodilation is getting the bronchioles to open wider using bronchodilator medications. Bronchodilator therapy is used for respiratory conditions that impact the airways in your lungs and prevent enough air from passing through them. The smooth muscles around the bronchioles (tubes that carry air) tighten and make the whole tube narrower. Depending on the disease, you may also have inflammation of the lining of the bronchioles or production of excess mucus.
When any of those things happen, your doctor may prescribe a medication to make the bronchioles dilate (widen).
Types of bronchodilators
Bronchodilator definition is based on the type of medications or how long they provide symptom relief.
Three major classes of medications are used as bronchodilators to treat the symptoms of chronic obstructive pulmonary disease (COPD), asthma or cystic fibrosis:
- Beta-2 agonist: Relaxes smooth muscles of the bronchioles. Sometimes combined with a corticosteroid to control other asthma symptoms.
- Anticholinergic: Dilates bronchioles, reduces excess mucus and reduces inflammation to help prevent bronchioles from narrowing.
- Xanthine derivatives such as theophylline: Dilates bronchioles and reduces excess mucus production.
Bronchodilators can also be described as long acting or short acting. Long-acting medicines are used every day to keep chronic breathing difficulties under control. Short-acting medicines are used occasionally for acute (sudden) breathing problems and are sometimes called rescue, quick-acting or reliever medicines. Your doctor may prescribe both types or only one type.
Beta-2 agonists and anticholinergic drugs may be short-acting or long-acting.
Theophylline is usually used as a long-acting medicine and is prescribed in the form of tablets or capsules. It’s used rarely as an intravenous (injected into a vein) short-acting liquid medicine to treat severe, sudden breathing problems.
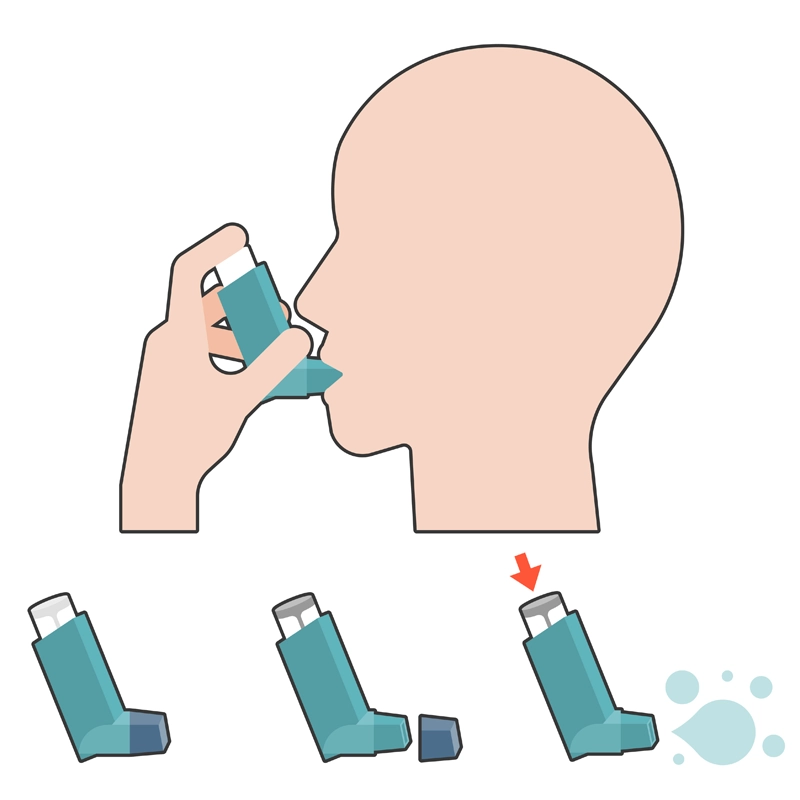
Administering bronchodilators for respiratory wellness
Bronchodilator therapy for COPD or other conditions can be prescribed as shots, tablets, liquids or inhalers (small canisters of medicine). Most doctors prescribe bronchodilators in the form of inhalers because inhalers make a precise dose of medication go directly to the lungs where it’s needed.
Inhaler usage depends on good timing of three steps:
- Exhale as completely as possible
- Put the mouthpiece of the inhaler in your mouth and press down on the canister while inhaling deeply
- Hold your breath as long as possible to keep the medication in your lungs
With practice, most people can learn to use an inhaler.
If you have trouble with the timing, your doctor may advise using a spacer between the mouth and the inhaler. Using a spacer allows the medicine to be held in an enclosed space so you can inhale more slowly. That helps the medicine get into your lungs instead of into your stomach.
Nebulizer treatments for bronchodilator therapy
Some bronchodilator medications can be delivered using a nebulizer, a device that changes liquid medications into a mist that you can inhale easily. Nebulizer treatments take longer than using an inhaler. They’re often used for younger children because they’re easier to use than inhalers.
Understanding potential side effects of bronchodilators
Common side effects of bronchodilators include trembling, nervousness, sudden heart palpitations and muscle cramps. Sometimes a bronchodilator will cause the muscles to spasm instead of relax. Allergic reactions are also possible.
There may be an adverse response to bronchodilator therapy delivered as a nebulizer treatment. Common side effects are rapid heartbeat, jitteriness or anxiety. Other side effects are:
- Throat irritation
- Headache
- Nausea
- Vomiting
Theophylline has more side effects than other bronchodilators, including rash, facial swelling, fainting, fever, seizures, unusual breathing or unusual heart rate. It’s used less often than other bronchodilators because many people have these side effects.
Always tell your doctor about any adverse effect of bronchodilator therapy.
Get care
We help you live well. And we’re here for you in person and online.
