Acute respiratory distress syndrome (ARDS)
When you have extreme shortness of breath and pain while breathing, it can be downright frightening. Acute respiratory distress syndrome (ARDS) is one of the conditions that can cause such symptoms. Advocate doctors and pulmonary specialists know what to do to improve your oxygen levels and deal with the underlying causes or conditions.
What is acute respiratory distress syndrome?
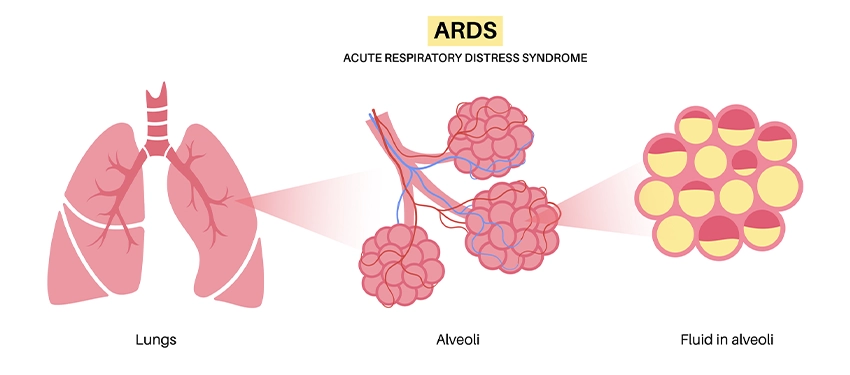
Acute respiratory distress syndrome (ARDS) happens after an injury to the lungs. The lungs have alveoli (tiny air sacs) where carbon dioxide is removed from blood and oxygen is added to the blood. When you have ARDS, the air sacs start to fill with fluid and can’t carry as much oxygen, which causes hypoxemia (low oxygen levels in blood).
Signs and symptoms of ARDS
There are a variety of potential ARDS symptoms. People commonly have shortness of breath that is so bad it’s distressing. This may lead to breathing faster and a faster heartbeat. You may also have pain while breathing. Some other acute respiratory distress syndrome symptoms are:
- Fingernails, lips or skin may look blue
- Coughing that produces phlegm
- Extreme fatigue
- Fever
- Low blood pressure
- Confusion
Understanding ARDS: causes & risk factors
The most common cause of ARDS is infections such as the flu, COVID or other viruses. Pneumonia and sepsis (an extreme, life-threatening reaction to an infection ) are other common causes. Other injuries and traumas that may lead to acute respiratory distress syndrome symptoms are:
- Trauma to the head, chest or other body parts
- Near drowning experience
- Blood transfusions
- Pancreatitis
- Inhaling harmful substances
- Reaction to some medicines
- Being on a heart-lung bypass machine or a ventilator
You may be more likely to develop ARDS if you are older or have:
- History of tobacco use
- History of alcoholism
- Chronic lung disease
- High-risk surgery
- Exposure to chronic air pollution
- Some genetic conditions
ARDS prevention strategies
You can lower your risk of ARDS by avoiding tobacco smoke, limiting alcohol, limiting exposure to pollution, and getting vaccinated for the flu, COVID and other infections.
Diagnosing ARDS: tests & procedures
If your doctor suspects you have ARDS based on your potential acute respiratory distress syndrome symptoms, one of the things they’ll do is listen to your breathing. Rattling, clicking or bubbling sounds may be signs you have ARDS.
The most common tests used for diagnosing ARDS effectively are a chest X-ray to look for fluid in the lungs and help identify if there has been a lung injury and a blood test to check levels of oxygen in the blood.
Your specialist may order a lung biopsy to help rule out heart disease and chronic lung disease because their symptoms are similar to ARDS symptoms.
ARDS treatment options: a comprehensive overview
The basics of treating ARDS are to repair the injury to the lungs, get enough oxygen into your blood so your body can work correctly and then wait for the lungs to heal.
Support for breathing with ARDS
You may receive extra oxygen from a tank linked to tubes resting in your nose. However, this kind of oxygen therapy is often not enough to resolve ARDS symptoms.
Your acute respiratory distress syndrome treatment may include noninvasive breathing support supplied using CPAP (continuous positive airway pressure) or BiPAP (bilevel positive airway pressure) machines. These devices are relatively low-risk options.
In case of severe breathing problems, you may be placed on an automatic ventilator to assist your breathing. Using a tight-fitting mask or an endotracheal tube inserted into your windpipe, the ventilator moves air or air enriched with oxygen into and out of your lungs.
Being on a ventilator for ARDS treatment may last for a week or two. Doctors will discontinue ventilator treatment as soon as possible because being on a ventilator increases the risk of getting pneumonia or having a collapsed lung. When it’s safe to stop using the ventilator, it’ll be done gradually to allow you to return to breathing on your own.
While on a ventilator, some people may be placed in a prone position (facing down) to help improve their breathing.
In some of our ICUs, extracorporeal membrane oxygenation (ECMO) may also be used for ARDS treatment. ECMO is a bypass procedure that uses a machine to circulate blood and oxygen through your body. ECMO treatment has some serious potential side effects, including bleeding, blood clots, infection, seizures or stroke. It can only be used for some people.
Medications for ARDS
When you’re on a ventilator or receiving ECMO treatment, you may receive sedation to help relieve shortness of breath, keep you from becoming agitated and lessen your body’s need for oxygen. Another acute respiratory distress syndrome medication that may be used is a paralytic medication to help you adjust to being on a ventilator. Both these types of medication will be used carefully to ensure they’re working as intended and not causing further problems.
People who have ARDS sometimes receive diuretic medications to help remove excess fluid from their bodies. Doctors are careful about using these medications as acute respiratory distress syndrome treatments because they sometimes lower blood pressure too much or cause kidney problems.
Antibiotics may be given to prevent or treat infections. Muscle relaxers may help prevent gagging or coughing while on a ventilator or they may reduce how much oxygen you need. Blood thinners may also be prescribed to prevent blood clots from forming.
Get care
We help you live well. And we’re here for you in person and online.
