Astrocytoma tumors
When you’re diagnosed with a brain tumor called an astrocytoma, you may need to start at the beginning to find out what it is. The answers depend on several things about the tumor including its size, its location and what the cells look like under a microscope. Your Advocate Health Care doctor will help you sort through the things you need to know to make informed decisions about your treatment.
What is an astrocytoma?
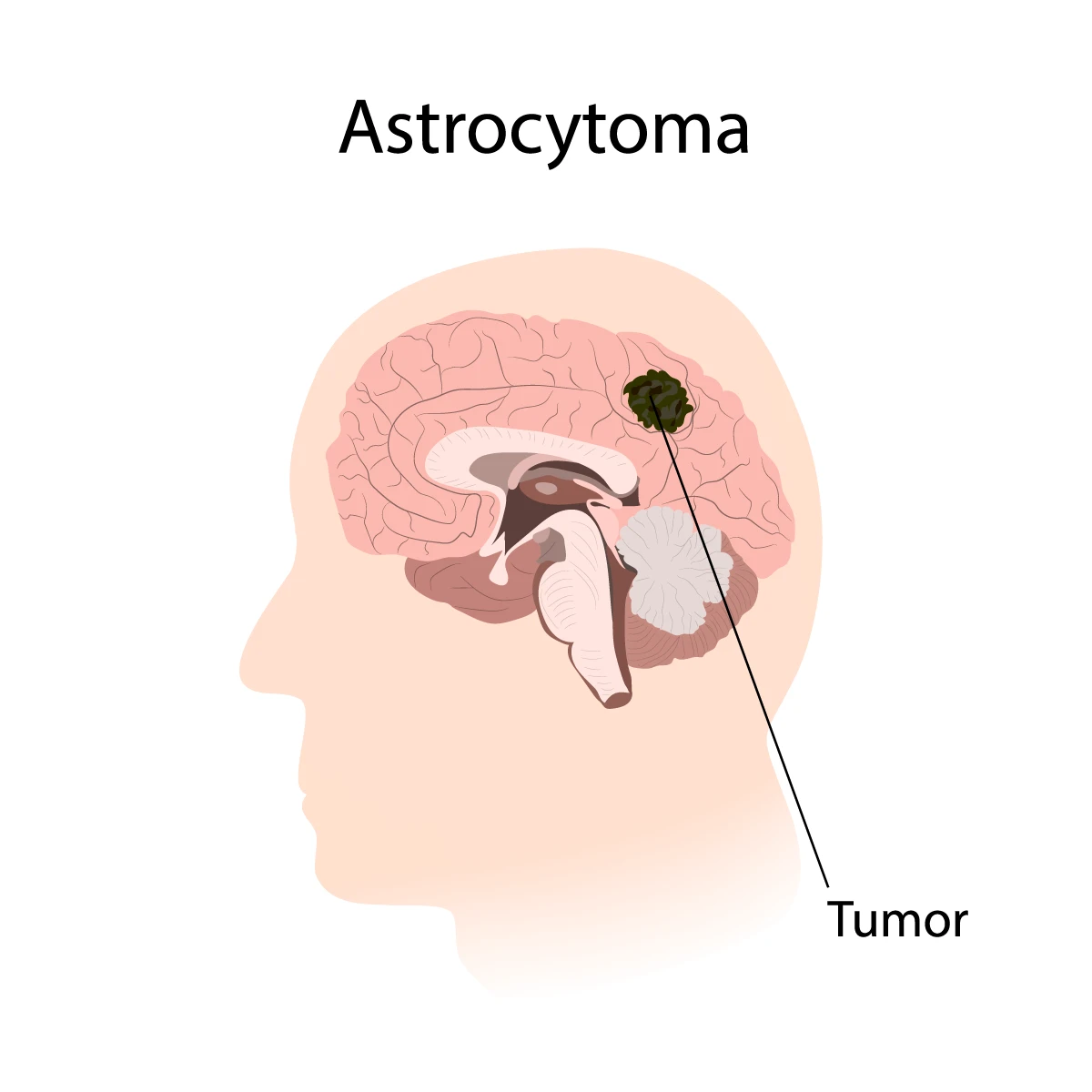
An astrocytoma is a type of primary brain tumor that starts growing from star-shaped cells called astrocytes. Most astrocytomas form in a part of the brain, with some starting in the spinal cord. They may be benign (noncancerous) or malignant (cancerous).
Astrocytomas can be life-threatening even if they’re benign because they may:
- Grow into other areas of the brain
- Be hard to reach and treat with surgery
Astrocytomas happen most often between the ages of 20-60. They happen more often in men than in women.
Astrocytoma risk factors
Having had treatment of the head and neck with radiation therapy during childhood increases the risk of developing an astrocytoma. These hereditary conditions may increase the risk of developing an astrocytoma:
- Li-Fraumeni syndrome
- Turcot syndrome
- Neurofibromatosis 1
- Tuberous sclerosis
Researchers continue to search for other risk factors.
Genetics & astrocytomas
Genetic testing of an astrocytoma tumor may be recommended for you. Research has uncovered some features of astrocytomas that have helped us understand the disease process.
Some types of astrocytoma tumors are related to mutations in certain genes. We’ve also discovered ways that the immune system gets turned off when it comes to astrocytoma cells. Researchers are confident that discovering a way to turn the immune system response back on will improve treatment of these types of astrocytomas.
Depending on what genetic testing shows us about your tumor, we may be able to recommend targeted therapy that attacks specific parts of cancer cells and doesn’t affect your healthy tissue.
Astrocytoma tumor types
Like other tumors, astrocytomas are evaluated in terms of what type they are. This is done through grading. Grading is based on details about the tumor. A biopsy (tissue sample) is taken, and the cells are examined under a microscope by a neuropathologist. The grade is assigned based on these findings:
- How abnormal the cells look compared to normal brain or spinal cord tissue
- How much the cells grow
- Whether there are new blood vessels within the tumor
Astrocytoma tumor grade 1
There are three kinds of grade 1 astrocytomas. Removing them is usually considered a cure.
- Pilocytic astrocytoma: Slow-growing tumor that doesn’t grow into surrounding areas of the brain. It’s the most common astrocytoma among children. Also known as Juvenile Pilocytic Astrocytoma (JPA).
- Pleomorphic xanthoastrocytoma (PXA): Rare, slow-growing tumor that may be related to seizures.
- Subependymal Giant Cell Astrocytoma (SEGA): Usually affects young people and is associated with tuberous sclerosis. Grows deep into the ventricles (fluid-filled spaces) of the brain and can cause swelling of the brain.
Astrocytoma tumor grade 2
Grade 2 astrocytomas are known as diffuse astrocytomas. The cells of these invasive tumors look abnormal under a microscope and there are more of them than normal. Surgery alone might not cure these tumors.
Astrocytoma tumor grade 3
Cells of anaplastic astrocytoma grow faster and look more abnormal under a microscope. They’re seen as more malignant than lower grade tumors and surgery is never enough to cure them.
Astrocytoma tumor grade 4
Also known as glioblastoma multiforme (GBM), grade 4 astrocytomas grow very quickly and are the most common cancerous brain tumor in adults. Glioblastoma cells appear very abnormal, form many new blood vessels and cause tissues to die.
Primary brain tumors vs. secondary brain tumors
Primary brain tumors are ones that start in the brain. Astrocytoma tumors usually affect only brain or spine tissues and don’t spread to other areas of the body.
Other brain and spine tumors may be secondary tumors, which means they’ve spread to the brain or spine from cancer that started in another part of the body. Another name for a cancer that spreads to a second site is metastatic tumor. Most metastatic brain tumors come from cancers of the colon, lungs, breasts, or kidneys, or from a melanoma (a type of skin cancer).
Astrocytoma tumor symptoms
Astrocytoma symptoms depend on where the tumors occur in the brain or spine. If the tumor grows in a space where there is more room to grow, it might not cause symptoms until it gets very large.
High grade astrocytomas may start to cause symptoms even when they’re still small because they cause more brain swelling, grow more quickly and destroy parts of the brain where they’re growing. Lower grade tumors don’t destroy brain tissue.
Common astrocytoma symptoms include:
- Persistent headaches
- Headaches which are worse in the morning or cause awakening from sleep
- Double or blurred vision
- Speech problems
- Problems with thinking, concentrating and making decisions
- Weakness in arms or legs
- New seizures
Astrocytoma diagnosis
When you see a doctor about potential astrocytoma symptoms, they’ll perform a physical and talk to you about your family medical history and symptoms. They’ll also ask questions and do tests to check your mental status, coordination, vision, ability to walk normally, and how well your muscles, senses and reflexes work.
Testing for astrocytoma
Your doctor will order imaging tests to identify what’s going on in your brain. A magnetic resonance imaging (MRI) scan will usually be the first test and it may be done both with and without a contrast dye injected into your bloodstream. High grade tumors tend to pick up more contrast dye than low grade tumors.
MRI spectroscopy (MRS) may also be used because it provides information about chemical levels in the tumor. Some chemicals are more abundant in tumors, and some are more common in normal brain tissues.
Functional MRI (fMRI) is another useful imaging tool. It’s used to see which parts of the brain are used when you’re asked to do things like moving your legs or talking. Using fMRI scans, your doctor can find out what functions the tumor is likely to affect, and it can help them plan any needed surgery.
Obtaining a tissue sample (biopsy) of a tumor is another important part of diagnosis. A neuropathologist will examine the tissue to identify whether it’s a primary or secondary tumor and what grade it is. Biopsies are often obtained at the same time as surgery to remove tumors to minimize the impact on the skull.
Astrocytoma treatment
Once an astrocytoma is diagnosed, cancer surgery will be the first step in your cancer treatment. Your surgeon will remove as much of the tumor as possible. This relieves the effects of swelling and makes any other astrocytoma treatments work better. For low grade benign or cancerous tumors, surgery may provide a cure.
In addition to surgery, you may be scheduled for radiation therapy, chemotherapy, immunotherapy, targeted therapy or some combination of these treatments.
Get care
We help you live well. And we’re here for you in person and online.
